Gingivitis is a very common condition among different societies and population groups. Many people around the world believe that gingivitis begins in early childhood and that 9-17% of children aged 3-11 years suffer from it, but it has been shown that the incidence increases significantly in adulthood, where it may reach 70-90%. The infection is more common in males than females, and it is also the most common chronic inflammatory condition among the elderly.
Some studies in Australia, Sweden, England, and Switzerland have indicated that 48-85% of children aged 3-6 years are affected by gingivitis.
What is Gingivitis
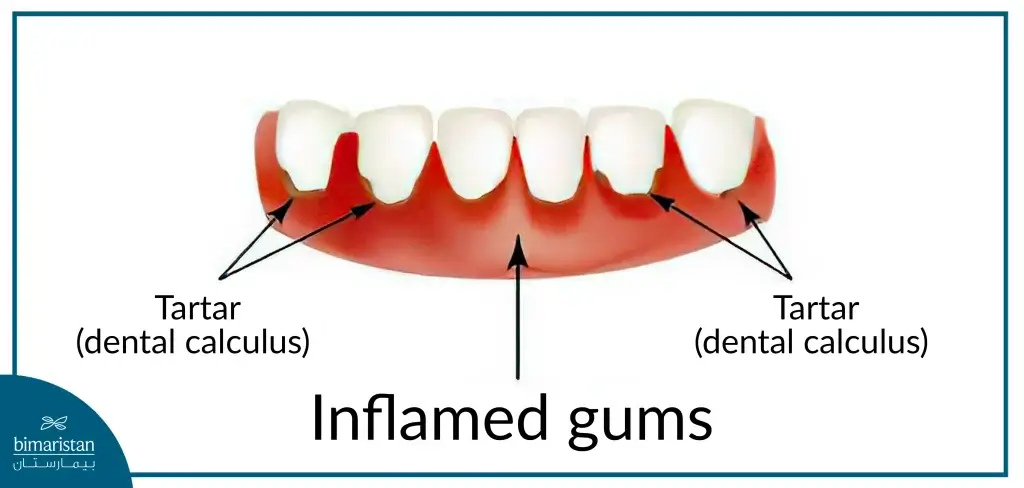
Gingivitis is an inflammatory condition that affects the gum tissues and is often caused by bacterial infections. The condition is confined to the soft tissue area of the gingival epithelium and connective tissue. There are various forms of gingivitis based on clinical presentation, duration of infection, severity of the condition, and the causative factor. However, chronic gingivitis caused by plaques (such as plaque or tartar) is the most common form.
Causes of Gingivitis
Bacterial infection is the most common cause of gingivitis, and it is involved in most other forms of gingivitis. There are many other causes that may lead to this condition, such as:
- Lack of daily oral and dental hygiene.
- Incomplete and inadequate removal of plaque.
- Allergic reactions.
- Poor nutrition.
- Tooth decay.
- Debilitating chronic diseases.
- Failure to conduct regular dental check-ups.
- Medication-related causes, such as anticoagulants, contraceptive pills, protease inhibitors, calcium channel blockers, vitamin A and its derivatives.

Gingivitis Symptoms
Most cases of mild gingivitis are asymptomatic for a long period, but they may cause various symptoms over time. The symptoms vary among affected individuals, with the most important ones being:
- Persistent bad breath that doesn’t go away even after brushing.
- Gums that bleed easily, especially when brushing teeth.
- Red, swollen, or puffy gums.
- Sensitivity to hot or cold foods.
- Pain when chewing food.

Treatment of Gingivitis
In chronic Inflammatory gums, brushing your teeth with fluoride toothpaste helps slow the progression of the disease and may aid in healing. Studies have shown that most electric toothbrushes provide additional benefits compared to manual brushing with a regular toothbrush. Brushing teeth daily, in addition to flossing, helps reduce plaque (tartar) and decreases bacterial counts. Recent studies indicate that brushing followed by rinsing with chlorhexidine or other mouthwashes may have better outcomes than brushing and flossing alone without using mouthwashes.
Patients with mild chronic gingivitis should be referred to a dentist, though not urgently, for plaque or tartar removal or to treat the underlying cause of the inflammation. Emphasizing the importance of maintaining regular oral hygiene is crucial, as it significantly helps in reducing the condition. Antibiotics and pain relievers may be needed in cases of severe gingivitis.
Quick Relief for Gingivitis
A topical oral anesthetic gel (Orajel), which often contains natural and synthetic ingredients that help numb the gums and relieve pain, can be used. Additionally, oral pain relievers like ibuprofen or acetaminophen (paracetamol) may be taken.
Medications for Gingivitis
Medications Provided Vary Depending on the Severity of the Condition and the Causative Factor
Treatment may rely on antiseptics, pain relievers, topical anesthetics, or antibiotics, and in some cases, a combination of more than one of the aforementioned medications may be used. To elaborate, we mention:
- Antiseptics: Such as 0.12% Chlorhexidine mouthwash (PerioGard), which has bactericidal activity. Studies have shown that it reduces the number of bacteria in the mouth.
- Pain Relievers: Such as acetaminophen (paracetamol), which is well-tolerated by most patients but should be used with caution in individuals with a history of drug allergies, or ibuprofen, which is used to relieve pain and helps reduce inflammation in the gums. Caution should be taken when using it in patients with a history of asthma or those suffering from peptic ulcers.
- Topical Anesthetics: Lidocaine anesthetic, which reduces the permeability of sodium ions in nerve membranes, leading to the inhibition of depolarization and preventing the transmission of nerve impulses.
- Antibiotics: Used to treat advanced chronic cases of inflammation and are not necessary for treating simple cases of inflammation. These antibiotics include penicillin (when there is no allergy to it), erythromycin as an alternative to penicillin, minocycline, doxycycline, or clindamycin. In fact, a dentist should be consulted before taking any antibiotic, as they will determine the best course of treatment based on the patient’s specific condition, taking into account important factors such as the patient’s medical history, allergies, and potential drug interactions before prescribing any antibiotic for treatment.
Antibiotic for Gingivitis
Several types of antibiotics can be used to treat gingivitis depending on patient-specific factors such as the severity of the condition, drug allergies, and others. These antibiotics include penicillin, erythromycin, minocycline, doxycycline, and clindamycin. These antibiotics work by killing both aerobic and anaerobic bacteria, thereby reducing and treating the inflammatory condition in the gums.
Gingivitis Mouthwash
There are many mouthwashes that may help reduce inflammation, including 0.12% Chlorhexidine mouthwash (PerioGard), which has been proven effective in reducing the severity of inflammation and maintaining gum health in numerous studies.
Treatment of Inflamed Gums in Turkey
Consulting a dentist is extremely important when it comes to gum inflammation. The dentist can provide the best treatment plan based on the patient’s specific condition and needs. Self-diagnosis or relying solely on antibiotics without professional guidance may not yield the desired results. Dentists can offer alternative treatments such as deep cleaning, tartar removal, scaling, root planning, or even surgical intervention in severe cases. They will address the underlying causes of the gum infection and help prevent its recurrence in the future.
Antibiotics may be prescribed if there is a necessity, as each individual’s case is unique; what works for one person may not work for another. Therefore, many cases may require personalized care specifically designed to meet the patient’s needs to effectively treat gum inflammation.
Types of Gingivitis
Gingivitis can be caused by several different factors, including:
Plaque-Induced Gingivitis
This is the most common cause of gingivitis. Plaque is a thin layer that forms on the surface of the teeth due to poor oral hygiene in general. If it is not removed regularly over time, it can harden and turn into what is known as tartar. Since plaque contains a large number of bacteria, which are the direct cause of inflammation, it significantly predisposes the gums to inflammation.
Gingivitis Due to Poor Nutrition
A deficiency in vitamin C can cause many gum diseases. It has been found that individuals whose diet heavily relies on large amounts of refined carbohydrates and a high level of fatty acids may be more prone to developing inflammatory processes in the gums.
Hormonal-Related Gingivitis
During pregnancy, significant changes occur in hormone levels in the blood, as well as an expansion of blood vessels, contributing to an exaggerated inflammatory response in the gum tissue, even in cases with small plaque accumulations. Some studies have indicated that estrogen levels determine the severity of plaque-induced gingivitis.
Hormonal changes occurring during puberty can affect how gum tissue responds when plaque accumulates on the teeth, leading to what is known as puberty gingivitis.
Drug-Induced Gingivitis
Many medications used to treat systemic conditions can cause gingivitis as a side effect, such as phenytoin (used for epilepsy), calcium channel blockers (used for angina and high blood pressure), anticoagulants and thrombolytic agents, oral contraceptives, protease inhibitors, and vitamin A and its analogs.
Complications of Gingivitis
If gingivitis is not treated appropriately, it can worsen and develop into a more severe form of gum disease called periodontitis. This can lead to many serious problems, such as abscesses, tooth loss, and gum recession.
How Gingivitis Treatment Is Followed Up at a Dental Clinic in Turkey
If tartar is present, home treatment for gingivitis may not be sufficient, and a visit to the dentist is necessary. The dentist will remove the plaque and tartar, a procedure known as scaling. This procedure may be uncomfortable, especially if there is extensive tartar buildup or the gums are very sensitive.
The dentist will also explain the importance of oral hygiene and how to brush and floss effectively, emphasizing its importance in preventing and treating gingivitis.
Follow-up appointments with repeated cleanings may be recommended if necessary.
Treating any damaged tooth also contributes to the ease of maintaining oral hygiene and establishing a healthy oral environment.
Some dental issues, such as poorly positioned teeth or improperly designed crowns or bridges, can make it difficult to remove plaque and tartar correctly, which can also lead to gum bleeding and irritation.
Gingivitis is often caused by poor oral hygiene and, if left untreated, can progress to more serious gum disease, leading to tooth loss and other health complications. Preventive measures such as regular dental checkups, good oral hygiene practices, and a balanced diet are essential in managing and preventing gingivitis. Early diagnosis and treatment are essential to reduce the risk of chronic gingivitis and maintain overall oral health. Awareness of the importance of oral health can significantly reduce the incidence of gingivitis and improve quality of life.
Resources:
